Does Medicare Cover External Female Catheters?
Key Takeaways
- Yes, Under Part B: Medicare Part B generally covers external female catheters as Durable Medical Equipment (DME) if they are deemed medically necessary.
- Medical Necessity is Mandatory: Coverage is provided for beneficiaries with permanent urinary incontinence as a non-invasive alternative to indwelling (Foley) catheters.
- Doctor’s Prescription Required: A face-to-face examination and a written prescription from a Medicare-enrolled doctor are essential.
- Quantity Limits Apply: Medicare has specific quantity limits for different types of female external collection devices, such as metal cups and collection pouches.
- Supplier Must Be Medicare-Approved: You must get your supplies from a Medicare-enrolled supplier to ensure coverage.

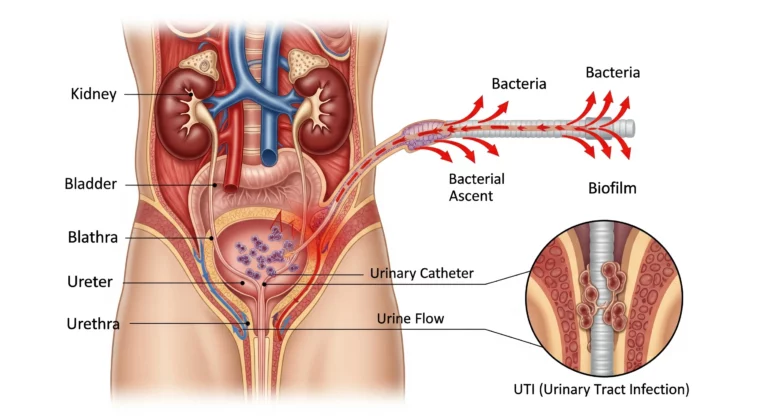
For many women living with urinary incontinence, external catheters offer a non-invasive and effective way to manage their condition and improve their quality of life. Compared to traditional indwelling catheters, which carry a higher risk of infection, or absorbent products that can cause skin irritation, external catheters provide a comfortable and hygienic solution. A common and crucial question for those on Medicare is whether this vital equipment is covered by their insurance.
The good news is that Medicare Part B does cover external female catheters, but it’s important to understand the specific rules and requirements to ensure you get the supplies you need.
How Medicare Covers External Catheters
External catheters and their related supplies are classified as Durable Medical Equipment (DME) under Medicare Part B. This means that to be eligible for coverage, the equipment must be medically necessary for a condition that is permanent or of long and indefinite duration (typically at least three months).
Coverage is typically provided under the following conditions:
- Permanent Urinary Incontinence: You must have a diagnosis of permanent urinary incontinence. This means the condition is not expected to be medically or surgically corrected within a reasonable timeframe.
- As an Alternative to Indwelling Catheters: Medicare covers external female catheters as an alternative to indwelling catheters. This means you generally cannot have coverage for an external catheter if you are also using an indwelling catheter.
- Doctor’s Order: Your treating physician must conduct a face-to-face examination and provide a detailed written order or prescription for the external catheters. This documentation must clearly state your diagnosis and explain why the equipment is medically necessary for your condition.
Step-by-Step Guide to Navigating Coverage

Here’s a breakdown of the steps you should follow to get your Medicare cover female external catheters.
Step 1: Visit Your Doctor
The process begins with a visit to your doctor. During this appointment, your doctor will assess your condition and determine if an external catheter is the most appropriate and medically necessary solution for your urinary incontinence. They will create a detailed record of your medical history, diagnosis, and the reason for the prescription. This documentation is crucial for justifying your need for the supplies.
Step 2: Get a Written Prescription
After your appointment, your doctor must provide a written prescription for the external catheters. This prescription should include:
- A clear diagnosis of permanent urinary incontinence
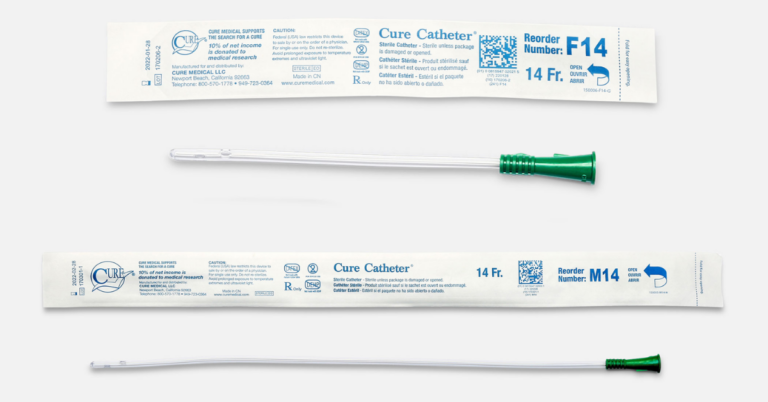
- The specific type of external catheter (e.g., pouch, meatal cup).
- The required quantity of supplies per day or month.
- The length of need for the equipment.
Step 3: Find a Medicare-Enrolled Supplier
It is absolutely essential to get your external catheters from a supplier that is enrolled in Medicare. If you use a supplier who is not, Medicare will not cover the cost, and you will be responsible for the full amount.
You can find a list of Medicare-enrolled suppliers on the official Medicare.gov website or by contacting 1-800-MEDICARE. When you contact a supplier, be sure to ask if they “accept assignment,” which means they agree to accept the Medicare-approved amount as full payment.
Step 4: Understand Your Costs and Quantity Limits
Like other DME, Medicare Part B covers 80% of the Medicare-approved amount for external catheters after you have met your annual Part B deductible. You will be responsible for the remaining 20% coinsurance.
Medicare has specific quantity limits for external female catheters, which are subject to change. For instance, Medicare’s Local Coverage Determinations (LCDs) state that generally, more than one metal cup per week or more than one collection pouch per day is not considered medically necessary. These limits are in place to prevent over-utilization, and any quantities exceeding these limits will require additional medical documentation to justify the need.
HCPCS Codes for External Female Catheters: Medicare uses specific Healthcare Common Procedure Coding System (HCPCS) codes for billing. Common codes for female external catheters include:
- A4327: Female external urinary collection device, meatal cup, each
- A4328: Female external urinary collection device, pouch, each
- E2001: Suction pump, home model, portable or stationary, electric, any type, for use with external urine management system. (This code applies to a system like PureWick, which includes a pump and wicking catheters)
By understanding the coverage criteria, working with your doctor and a Medicare-enrolled supplier, and being aware of quantity limits, you can successfully navigate the process of getting your external female catheters covered by Medicare.
FAQs Medicare & External Female Catheter Coverage
Q: Does Medicare cover external female catheters?
A: Yes, Medicare Part B covers external female catheters as Durable Medical Equipment (DME) if they are deemed medically necessary by a doctor for permanent urinary incontinence.
Q: What is "medically necessary" for external female catheter coverage?
A: To be considered medically necessary, you must have a diagnosis of permanent urinary incontinence that is not expected to be corrected by surgery or medical treatment within a reasonable timeframe (usually at least three months). The catheter is covered as an alternative to an indwelling catheter.
Q: What steps do I need to take to get my external catheters covered?
A: The process involves a few key steps:
- See Your Doctor: Have a face-to-face appointment with your doctor to get an official diagnosis and discuss your needs.
- Get a Prescription: Your doctor must provide a detailed written prescription or order.
- Choose a Supplier: Find a supplier that is enrolled in and “accepts assignment” from Medicare.
Q: What are the common quantity limits for external female catheters?
A: Medicare has specific quantity limits to prevent over-utilization. Typically, coverage is limited to one meatal cup per week or one collection pouch per day, although these limits can be exceeded with additional medical documentation from your doctor to justify the need.
Q: How much will I have to pay for external female catheters with Medicare?
A: After you meet your annual Medicare Part B deductible, Medicare will cover 80% of the Medicare-approved amount. You are responsible for the remaining 20% coinsurance.
Q: What are the HCPCS codes for external female catheters?
A: Common HCPCS codes used for billing external female catheters include:
- A4327: Female external urinary collection device; meatal cup.
- A4328: Female external urinary collection device; pouch.
- E2001: Suction pump, home model, for use with an external urine management system (for wicking systems like PureWick)